Connect With Us
Blog
Items filtered by date: December 2020
Exploring the Root Causes of Cracked Heels

Cracked heels, a common foot woe, often result from a combination of environmental, lifestyle, and health factors. Dry skin, exacerbated by insufficient hydration, is a leading culprit, and exposure to harsh weather conditions, such as cold or dry air, can strip the skin of its natural moisture. Prolonged standing or walking on hard surfaces may contribute to pressure on the feet, leading to calluses and eventual cracking. Inadequate foot care, including infrequent moisturizing and neglecting proper exfoliation, can make the problem worse. Additionally, conditions such as obesity and diabetes may compromise skin health, increasing vulnerability to cracked heels. Footwear choices also play a role, as open-back shoes or sandals expose the heels to friction and dryness. Recognizing and addressing these underlying causes is essential for effective management. If you have developed cracked heels, it is strongly suggested that you visit a podiatrist who can effectively treat this condition, which may include prescribed medication.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Leonard Talarico, DPM from Georgia. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Causes of Athlete's Foot and Ways to Avoid It

Athlete's foot, a common fungal infection, can cause discomfort and itching, urging us to delve into its origins and effective prevention strategies. This condition thrives in warm, damp environments, making communal spaces like locker rooms, swimming pools, and shared showers breeding grounds. Direct contact with the fungus through contaminated surfaces or by sharing items such as towels and shoes facilitates its spread. Prevention begins with practicing good hygiene, including thorough drying between toes and keeping feet clean. Opting for breathable footwear and moisture-wicking socks helps maintain a dry environment, discouraging fungal growth. Regularly changing socks and allowing shoes to air out are essential habits to practice. Additionally, avoiding walking barefoot in public areas further reduces the risk of exposure. Swift attention to any signs of infection, such as redness or scaling, is pivotal for early intervention. If you have developed athlete’s foot, it is strongly suggested that you confer with a podiatrist who can effectively treat this condition, which may include prescribing medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Leonard Talarico, DPM from Georgia. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stages of Gout

Gout is a type of joint problem caused by the formation of tiny crystals. It happens when your body makes too much uric acid, or your kidneys do not get rid of it efficiently. This uric acid is a leftover from breaking down certain foods. When uric acid levels get too high, it turns into crystals that cannot dissolve and remain in your tissues, causing inflammation. Your body's defense cells try to absorb these crystals, but they may become damaged as a result of how sharp they are. Gout is more common in men and often shows up after age 30 or in women after menopause. Gout has four stages. The first stage involves high uric acid with no symptoms. The second stage includes painful joint attacks The third stage is generally pain-free periods between attacks. The fourth stage consists of severe gout with lumpy deposits that are known as tophi. During a gout attack, you will experience severe pain, redness, swelling, and warmth in the joint. The big toe is a common spot for gout, and over time, untreated gout can harm your joints. In severe cases, surgery may be needed if the joint damage is extensive. Gout can be diagnosed by examining joint fluid or having X-rays taken. If you believe you have gout, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and treatment.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Leonard Talarico, DPM from Georgia. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Podiatric Care For Morton’s Neuroma
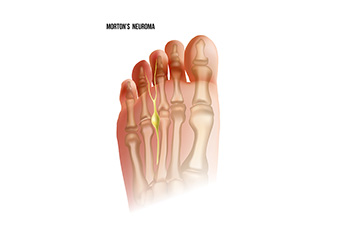
Morton's neuroma is a condition that affects the forefoot. Despite its name, it is not a true neuroma but rather a result of nerve fibrosis. This fibrosis occurs due to pressure or repetitive irritation, resulting in the thickening of the digital nerve, typically found in the third or second intermetatarsal space. Managing Morton's neuroma involves various treatment options. Orthotics, which are custom-made shoe inserts, can provide relief by altering foot mechanics and reducing pressure on the affected nerve. Steroid injections can also be administered to alleviate inflammation and pain. In more severe cases, surgical excision may be necessary, typically performed through a dorsal approach. Successful management of Morton's neuroma relies on several critical factors. If you feel you have Morton’s neuroma, it is suggested that you schedule an appointment with a podiatrist. A thorough examination is essential to accurately diagnose and treat this condition.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Leonard Talarico, DPM of Georgia. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Do Your Child's Feet Hurt?
Managing a Broken Foot

Managing a broken foot requires immediate attention and a structured treatment plan to ensure proper healing. Immobilization of the foot is often necessary to prevent further injury, and this may involve using splints, casts, or walking boots. The type of fracture dictates the specific immobilization method. Pain relief is an important aspect of management. In some cases, particularly for more complex fractures, surgery may be necessary to realign and stabilize the bones. Following immobilization, the patient usually needs to limit weight bearing on the injured foot, sometimes with the aid of crutches or a scooter. A podiatrist will establish a timeline for the gradual reintroduction of weight-bearing activities. If you have broken your foot, it is suggested that you make an appointment with a podiatrist as quickly as possible, and follow their instructions to prevent re-injury in addition to proper bone healing.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Leonard Talarico, DPM from Georgia. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020