Connect With Us
Blog
Items filtered by date: December 2020
Managing Gout with Exercise

Gout, a form of arthritis caused by the buildup of uric acid crystals in the joints, can be debilitating and painful. However, incorporating regular exercise into your routine can help manage symptoms and improve overall well-being. Low-impact activities such as walking, swimming, and cycling are gentle on the joints and can help reduce inflammation and stiffness associated with gout. It is beneficial to aim for at least 30 minutes of moderate exercise most days of the week to reap the benefits. Strength training exercises focusing on the muscles surrounding the affected joints can help improve stability and support, reducing the risk of gout attacks. Additionally, maintaining a healthy weight through regular exercise and a balanced diet can help decrease uric acid levels in the body, potentially preventing gout flare-ups. By incorporating regular exercise into your lifestyle, you can effectively manage gout and enjoy improved joint health and mobility. If you have developed gout, it is strongly suggested that you are under the care of a podiatrist who can help you manage this painful condition, which may include gentle exercise.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Leonard Talarico, DPM from Georgia. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
Hammertoe and Its Causes

Hammertoe is a foot deformity characterized by an abnormal bending of the toe joints, causing the affected toe to resemble a hammer or claw. This condition typically affects the second, third, or fourth toes. It results from an imbalance in the muscles, tendons, and ligaments that control toe movement. Tightening of the ligaments and tendons, often due to wearing ill-fitting shoes with narrow toe boxes or high heels, can force the toes into a bent position over time. Additionally, genetic predisposition, foot structure abnormalities, and underlying conditions like arthritis or nerve damage can contribute to the development of hammertoes. As the condition progresses, individuals may experience pain, discomfort, corns, or calluses on the affected toes, making it difficult to wear shoes comfortably. Early intervention through proper footwear, toe exercises, orthotic devices, and, in severe cases, surgical correction can help alleviate symptoms and prevent complications associated with hammertoe. If you have hammertoe, it is suggested that you seek guidance from a podiatrist for an appropriate diagnosis and management of this condition.
Hammertoes can be a painful condition to live with. For more information, contact Leonard Talarico, DPM of Georgia. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
It's Time for Beautiful Feet
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
What Feet Can Reveal About Overall Health

Feet, often overlooked, hold valuable clues about our overall health and well-being. Various signs and symptoms manifesting in the feet can serve as indicators of underlying health conditions. For instance, changes in skin color or texture may signify circulatory issues or skin disorders, while brittle or discolored toenails can hint at fungal infections or nutritional deficiencies. Swelling in the feet and ankles may be from fluid retention, heart problems, or kidney issues. Furthermore, nerve damage in the feet can be an early sign of conditions like diabetes or neuropathy. Additionally, foot pain and discomfort can result from musculoskeletal problems, arthritis, or wearing improper footwear. Regularly inspecting and caring for our feet can help detect potential health concerns early and facilitate timely intervention. By paying attention to the signals our feet convey, we can take proactive steps to safeguard our well-being and maintain optimal health. If you are experiencing any foot pain or discomfort, it is strongly suggested that you visit a podiatrist who can help you with relief and treatment solutions.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Leonard Talarico, DPM from Georgia. Our doctor will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Handle a Long Work Day on Your Feet
In 2014, the American Podiatric Medical Association surveyed 1,000 American adults and found that half of all respondents lived with foot pain. Fortunately, there are ways to avoid foot problems such as following a daily footcare routine and wearing proper footwear at work.
If you have a job that requires you to be on your feet, it is best that you do not wear flat sole shoes. Your heel should be slightly elevated (less than 2 inches, but at least ¼-inch) if you are going to be standing for a prolonged period. You should also make sure that the shoes you wear are not too small. Tight shoes may cut off circulation to your feet, which will result in pain and blisters. It is always best to purchase fitted shoes later in the day, because the feet tend to swell as the day progresses. It may also be helpful to buy shoes a half size larger if you plan on wearing custom orthotics or arch supports.
Your muscles may become stiff when you are constantly standing up. It is important to take breaks every hour to stretch and relax. One tip is to perform calf raises, because this exercise will help improve your circulation. To perform this stretch, you first need to stand on the edge of a step with your abdominal muscles pulled inward. You then need to grip the step with the balls of your feet with your heels hanging over the edge. Next, try to raise your heels above the step by a few inches while standing on your tiptoes; hold this pose for a second. You should then lower your heels back even to the platform. These calf raises should be done ten times for full effectiveness.
You should also take care of your feet while you are at home. One of the best ways to prepare your feet for a long day of work is to soak them in ice water. Doing so for 20 minutes will help fight the swelling and inflammation that results from being on your feet at work.
Nevertheless, if you are experiencing pain in your feet, you should seek help from your podiatrist. Your doctor will help treat any ailments you may have in addition to helping you prevent any other ailments from developing in the future.
Pain Caused by Working on Your Feet

If you are experiencing foot pain after a long day on your feet at work, you are not alone. The fatigue from standing all day can lead to discomfort, but if the foot pain persists, it may indicate more serious issues such as plantar fasciitis or heel spurs. Several factors contribute to foot pain and fatigue after working, including having inadequate support in your shoes, particularly if you are on hard surfaces like concrete or tile. Uneven pressure distribution within the foot and poor circulation can make the problem worse, leading to swelling and further discomfort. Additionally, existing foot conditions like bunions and Morton’s neuroma can intensify the pain. To alleviate foot pain after work, consider investing in supportive footwear with cushioned soles, taking breaks to stretch and walk, and wearing compression socks if circulation is an issue. Incorporating foot exercises and stretches into your daily routine can also help improve foot strength and flexibility, reducing the likelihood of pain. If foot pain persists, it is suggested that you schedule an appointment with a podiatrist for proper diagnosis and treatment options.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact Leonard Talarico, DPM from Georgia. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
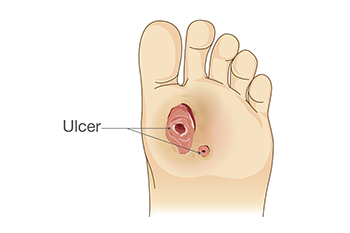
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Understanding Slow Wound Healing in Diabetic Patients
Wound healing is a complex process that can be significantly delayed in diabetic patients due to various physiological factors. High blood sugar levels characteristic of diabetes can impair the body's ability to repair damaged tissue by disrupting the function of immune cells, such as macrophages and neutrophils, responsible for combating infections and initiating the healing process. Additionally, diabetes often leads to poor circulation, reducing the delivery of oxygen and nutrients to the site of the wound, which is essential for tissue regeneration. Peripheral neuropathy, another common complication of diabetes, causes nerve damage and diminishes sensation in the extremities, making it difficult for patients to detect injuries and ulcers in their early stages. Furthermore, compromised immune function and increased susceptibility to infections further hinder the healing process. Managing blood sugar levels, maintaining proper foot care, and seeking prompt medical attention for wounds are crucial steps in minimizing the risk of complications and promoting effective wound healing in diabetic individuals. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can provide you with effective wound prevention tips, in addition to helping you manage this serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Leonard Talarico, DPM from Georgia. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020